A sudden wave of intense abdominal pain could be more than just a bad meal. It could be a warning sign of Pancreatic inflammation, a potentially life-threatening inflammation of the pancreas that requires urgent medical attention.
Thousands grapple with this condition annually, often mistaking it for less serious ailments. But ignoring these symptoms can lead to severe complications.
How can you tell if your abdominal pain signals pancreatitis? What steps should you take if you suspect you have it? Let’s find out!
Get Emergency Care for Pancreatitis
Understanding Pancreatitis

Pancreatitis is inflammation of the pancreas, causing swelling and pain that often radiates from the abdomen to the back. Your pancreas, about the size of your hand, sits between your stomach and spine.
This vital organ plays a crucial role in digestion and blood sugar regulation. It produces digestive enzymes (such as amylase) and hormones (like insulin) and transfers these to the small intestine via the pancreatic duct.
Inflammation is a response from your immune system to injury, intended to help heal damaged tissues. In the case of Pancreatic inflammation, the inflammation is often due to gallstones blocking the pancreatic duct or excessive alcohol consumption.
Acute Pancreatitis vs. Chronic Pancreatitis
Acute pancreatitis is a temporary condition caused by brief pancreatic injury. Most cases resolve within a few days with appropriate supportive care, including rest, hydration, and pain management. However, in severe cases, acute Pancreatic disorder can lead to serious health complications.
Pancreatic disease is a long-term, progressive illness resulting from ongoing pancreatic damage. Over the years, this condition can lead to permanent harm to the pancreas. Persistent inflammation results in scarring of pancreatic tissues (known as fibrosis), which impairs the pancreas’s ability to produce digestive enzymes and hormones.
Pancreatitis Symptoms

Symptoms of Acute Pancreatitis
- Severe Abdominal Pain
- Nausea and Vomiting
- Fever
- Fast Heart Rate
- Rapid, Shallow Breathing
- Tenderness in the Abdomen
- Swollen Abdomen
Chronic Pancreatitis Symptoms
- Persistent Abdominal Pain
- Indigestion
- Loss of Appetite
- Unintended Weight Loss
- Fatty, Oily Stools
- Lightheadedness
Acute Pancreatic disorder is often more intense and may have a sharp, penetrating sensation. Your abdomen might be tender when touched. In contrast, chronic Pancreatic inflammation involves pain that can vary in intensity. It may come and go, but usually does not completely resolve. You might experience increased pain after eating, and for some individuals, the pain may be continuous.
Notably, symptoms of Pancreatic inflammation and general abdominal pain can often overlap. If you or a loved one is experiencing abdominal pain, especially if it’s severe or persistent, consult a healthcare professional immediately for an accurate diagnosis and appropriate treatment.
Comprehensive Guide to Abdominal Pain
Pancreatitis Causes
The leading causes of Pancreatic disorder are:
- Gallstones: When a gallstone blocks the common bile duct, it can obstruct the flow of pancreatic juices. This blockage causes the digestive enzymes to accumulate and start digesting the pancreas itself, resulting in gallstone Pancreas inflammation.
- Heavy Drinking: Excessive alcohol consumption is a significant cause of pancreatitis. While the precise mechanism is not fully understood, it’s known that the toxic byproducts of alcohol or the activation of digestive enzymes within the pancreas can lead to inflammation. Heavy drinking is estimated to account for approximately half of all cases of both acute and chronic Pancreatic disease.
Other less common causes include:
- Infections: Certain viruses can lead to pancreatitis.
- Autoimmune Diseases: Conditions where the immune system attacks the pancreas, such as autoimmune Inflamed pancreas.
- Genetic Mutations: Inherited genetic conditions can cause pancreatitis.
- Cystic Fibrosis: Complications from this genetic disorder can affect the pancreas.
- High Triglyceride Levels: Elevated levels of triglycerides in the blood can trigger Inflamed pancreas.
- High Calcium Levels: Excessive calcium in the blood (hypercalcemia) can contribute to inflammation of the pancreas.
- Ischemia: Reduced blood flow to the pancreas can lead to inflammation.
- Cancer: Tumors in the pancreas or nearby organs can cause Inflamed pancreas.
- Trauma: Physical injury to the pancreas can result in inflammation.
- Medications: Some drugs can irritate the pancreas and trigger inflammation.
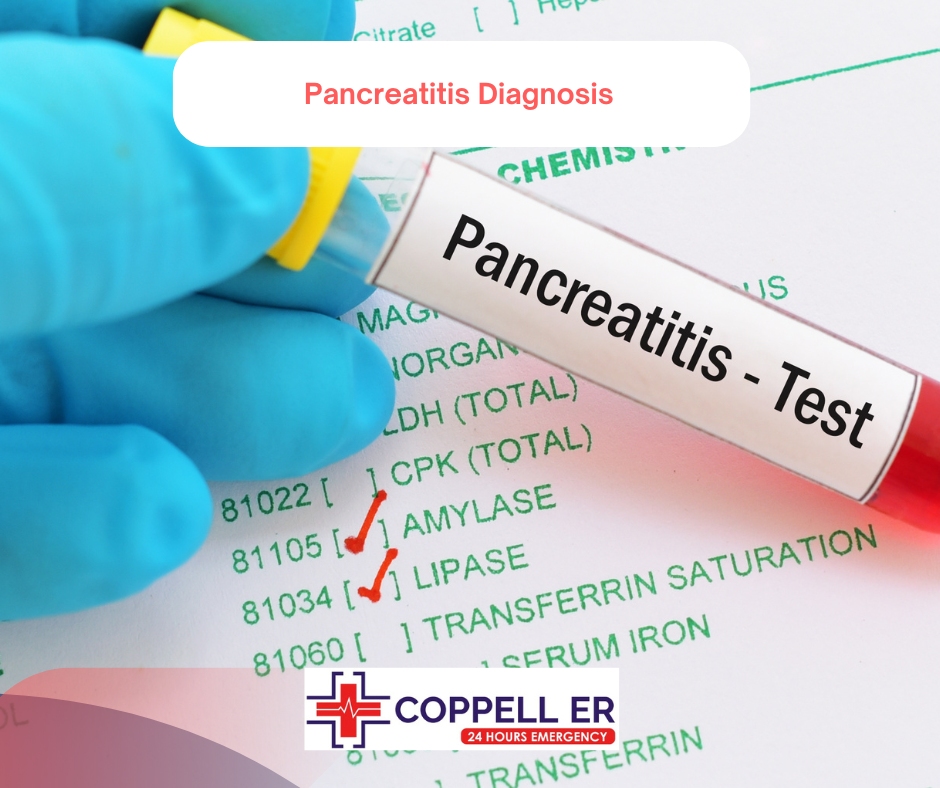
Pancreatitis Diagnosis
Clinical Evaluation
The first step in diagnosing Pancreatic inflammation is a detailed medical history and physical examination. Your doctor will ask about your symptoms, such as abdominal pain, nausea & vomiting, and changes in bowel movements. They will also consider risk factors like alcohol consumption, certain medications, or a history of gallstones.
Laboratory Tests
Several blood tests are commonly used to diagnose pancreatitis and assess its severity:
- Amylase and Lipase Levels: Elevated levels of these digestive enzymes can indicate Pancreas inflammation.
- Complete Blood Count (CBC): This test helps identify signs of infection or inflammation.
- Liver Function Tests: These can help determine if gallstones are causing the Pancreatic disorder.
Imaging Tests
Imaging tests are crucial for visualizing the pancreas and detecting any complications or underlying causes:
- Abdominal Ultrasound: This test helps identify gallstones or other abnormalities in the abdominal organs.
- CT Scan: A computed tomography scan provides detailed images of the pancreas and can reveal inflammation, fluid collections, or other complications.
- MRI: Magnetic resonance imaging may be used if CT results are inconclusive or if there is a need for additional detail.
Endoscopic Procedures
In some cases, endoscopic techniques are used to diagnose and manage pancreatitis:
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure involves inserting a flexible tube with a camera through the mouth to examine the bile and pancreatic ducts. It can also be used to remove gallstones or place stents.
Additional Tests
Depending on the underlying cause of pancreatitis, further tests may be needed:
- Genetic Testing: Used to identify inherited forms of Inflamed pancreas.
- Pancreatic Function Tests: Evaluates the pancreas’s ability to function and produce digestive enzymes.
- Glucose Test: Assesses whether the pancreas is producing insulin effectively.
- Stool Elastase Test: Determines if the pancreas is generating adequate digestive enzymes.
- Fecal Fat Analysis: Detects excess fat in the stool, which can indicate fat malabsorption.
At Coppell ER, our state-of-the-art medical laboratory is equipped to perform all essential blood tests and diagnostic procedures needed for a rapid and accurate diagnosis of pancreatitis.
Pancreatitis Treatment
Treatment Overview
- Hospitalization: Most cases of pancreatitis require hospitalization for intensive care and close monitoring
- Fasting: Fasting from food and drink is usually necessary to allow the pancreas to rest and heal. Nutritional support may be provided through an IV or feeding tube.
- Pain Relief: Effective Inflamed pancreas pain relief involves using medications to manage discomfort.
- Hydration: IV fluids help maintain hydration and overall health.
- Treating the Cause: Addressing the underlying cause, such as gallstones or alcohol consumption, is crucial for effective treatment. This may include procedures like gallbladder removal or alcohol cessation programs.
- Antibiotics: If an infection is present, antibiotics may be prescribed.
Pancreatitis Management
- Lifestyle Changes: For pancreatitis management, avoiding alcohol, quitting smoking, and following a low-fat diet are key. These lifestyle adjustments help prevent flare-ups and complications.
- Enzyme Supplements: Pancreatic enzyme replacements assist with digestion and help manage symptoms.
- Insulin Therapy: If the condition affects insulin production, insulin therapy may be required.
- Nutritional Support: A dietitian can provide guidance on maintaining a balanced diet and preventing malnutrition.
- Surgery: In severe cases, surgical intervention may be necessary to remove damaged tissue or drain fluid collections.
If you experience severe abdominal pain, persistent nausea, or other significant symptoms, it’s important to seek medical attention promptly. Regular follow-up is essential for effective pancreatitis management and to prevent complications.
Request an Appointment for Pancreatitis Evaluation Now
FAQs
Is pancreatitis very serious?
Yes, pancreatitis can be very serious, especially if left untreated. It can lead to severe complications like organ failure, infections, or chronic pain, and in severe cases, it can be life-threatening.
Can you live a long life with pancreatitis?
Yes, many people with pancreatitis can live a long life with proper management and treatment.
Can pancreatitis go away without hospital?
Mild cases of pancreatitis may improve with outpatient care and lifestyle changes, such as avoiding alcohol and following a special diet. However, severe cases often require hospitalization for intensive treatment and monitoring to prevent complications.
Can you fully recover from pancreatitis?
Yes, most individuals fully recover from pancreatitis, though some may experience recurring episodes.